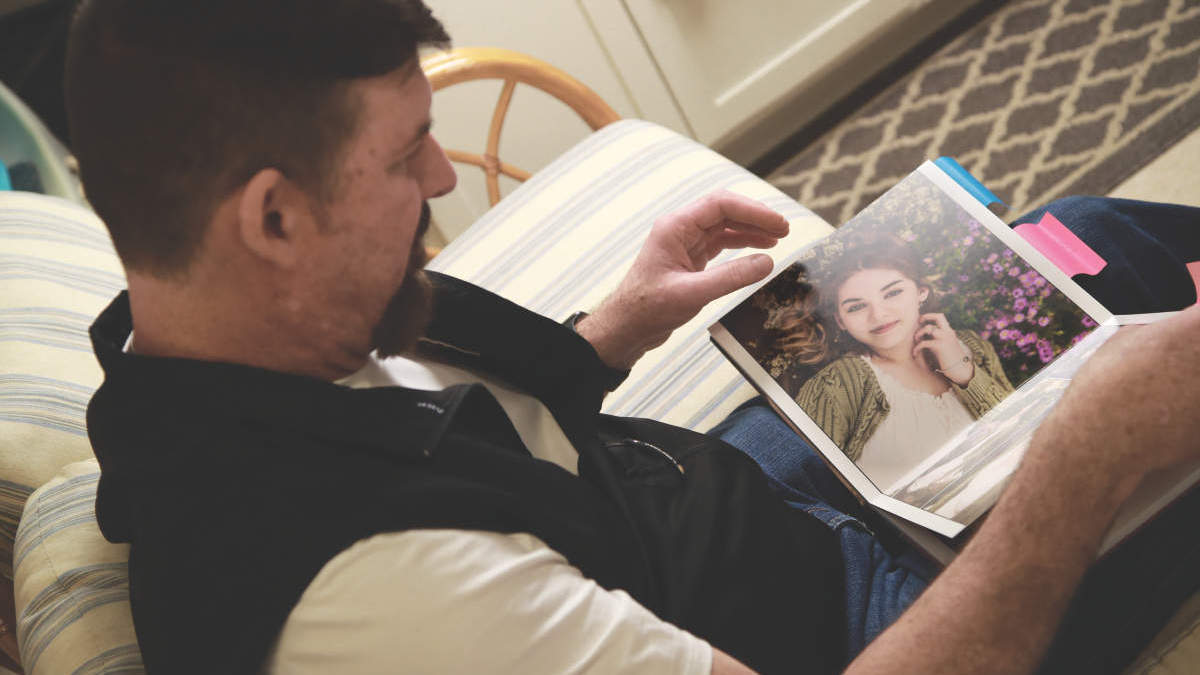
The first child cured of leukemia with CAR-T cell therapy set off a revolution in treating pediatric cancer. The therapy has since helped thousands of patients live longer. But for her parents, Tom and Kari Whitehead, getting their daughter back wasn’t enough. They tirelessly continue to help cancer patients access treatment and raise funds for research to help more patients achieve long-term remission.
Standard treatment had failed our daughter Emily twice. She had cancer for the third time and they were ready to send us home on hospice.
Tom Whitehead
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Emily was able to become the first child in the world with her immune system trained to beat her cancer with CAR T cells.
Tom Whitehead
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Since Emily got better, we've been doing whatever we can to pay it forward to help other families have the same outcome that we've had.
Tom Whitehead
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
When you save a child, you save a family.
Tom Whitehead
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
Co-founder, Emily Whitehead Foundation & Lead Lineman at Penelec
May 2023



